September 7, 2016
Back to School: Your Post-MACRA Study Guide for QPP Success
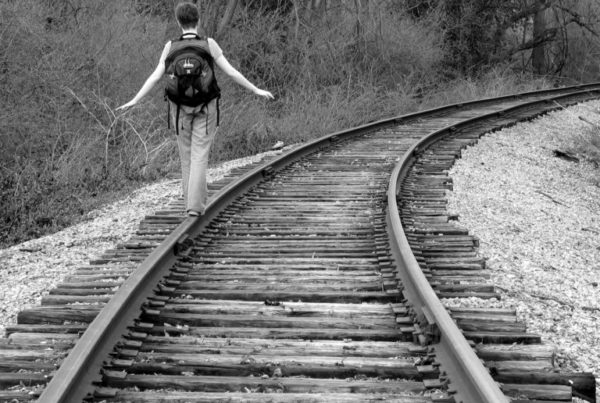
Back to school. That phrase prompts memories of making new friends (and catching up with old friends); carts full of notebooks, binders and pens; new classes; and, of course, abject terror. As the summer sun sets on PQRS, the Value Modifier (VM) and Meaningful Use (MU), it’s time for all of us to get into back-to-school mode, take the lessons we’ve learned and build on them for future success. Unfortunately, however, there’s an added challenge. Rather than having a season off to rest, regroup and ease into the new fall schedule, the transition from old programs to new is immediate…
Read More